opioid
Current sort has key articles at the top. Click on "Article Date" to sort by date, click on specific "tag" to view all articles in that category.
| Title/Link | |
|---|---|
|
The Pharming of Cannabis: Have We Not Learned the Lesson from the Overuse of Opioids? 11/14/2022 |
opioid, 2023 Presentation Dr Berry |
|
Marijuana Legalization and Opioid Deaths 02/16/2022 |
These results indicate that legal medical marijuana, particularly when available through retail dispensaries, is associated with higher opioid mortality. The results for recreational marijuana, while less reliable, also suggest that retail sales through dispensaries are associated with greater death rates relative to the counterfactual of no legal cannabis. fatal, opioid, Fatalities, Medical, 2023 Presentation Dr Berry |
|
Cannabis and the Gateway Drug Theory 10/15/2021 |
CANNABIS AND THE GATEWAY DRUG THEORY: CORRELATION OR CAUSATION – WHERE DOES THE EVIDENCE POINT? gateway, pathway, Johnnys Ambassadors, opioid |
|
Is marijuana use associated with decreased use of prescription opioids 02/17/2020 |
CONCLUSIONS: opioid, drivers, PubMed |
|
Understanding Opioid Use Disorder (OUD) using tree-based classifiers 02/12/2020 |
Machine learning can accurately predict adults at risk for OUD, and identify interactions among the factors that pronounce this risk. Curbing early initiation of marijuana may be an effective prevention strategy against opioid addiction, especially in high risk groups. OUD, opioid |
|
Reducing the risks of distortion in cannabis research 09/08/2019 |
But the lives of vulnerable people may be put at risk when science is distorted for corporate or ideological ends. As noted, several USstates responded to the much-hypedoriginal study of cannabis and opioid overdosesby authorizing the use of medical cannabis to treat heroin-addicted individuals. Advice that opioid users should use medical cannabis toreplace opioid agonist therapies (e.g., methadone, buprenorphine) poses significant risk because abrupt cessation of these medications dramatically increases the risks of an overdose death if users return to opioid use Research, Medical, risks, opioid |
|
Medical and non-medical cannabis use and risk of prescription opioid use disorder: Findings from propensity score matching. 08/01/2019 |
DISCUSSION AND CONCLUSIONS: opioid |
|
Does Medical Cannabis Reduce Use of Prescription Opioids? 02/06/2019 |
Is the solution to the opioid epidemic as simple as the legalization of medical cannabis? Commenting on the Bachhuber et al. analysis (1), Finney et al. (4) cautioned that an ecological fallacy may be present—individuals using medical marijuana could have elevated overdose mortality rates even though there is a state-level reduction. They contended that a prospective study of individual pain patients was necessary to assess relationships between cannabis use, use of opioid medications, and other substance use (4). olfson, opioid |
|
Why Marijuana Will Not Fix the Opioid Epidemic 01/20/2019 |
In 2017 Colorado had a record number of opioid overdose deaths from any opioid, including heroin and Colorado has had a medical marijuana program since 2001.6
There is currently a large and growing body of evidence showing that cannabis use increases, rather than decreases non-medical prescription opioid use and opioid use disorder, based on followup of more than 33,000 people.19 Concurrent use of cannabis and opioids by patients with chronic pain appears to indicate a higher risk of opioid misuse.20 Closer monitoring for opioid-related aberrant behaviors is indicated in this group of patients and it suggests that cannabis use is a predictor of aberrant drug behaviors in patients receiving chronic opioid therapy. opioid, Finn, ncbi |
|
increased risk of prescription opioid misuse 09/13/2018 |
New research suggests that marijuana users may be more likely than nonusers to misuse prescription opioids and develop prescription opioid use disorder. The study was conducted by researchers at the National Institute on Drug Abuse (NIDA), part of the National Institutes of Health, and Columbia University. opioid |
|
DFAF: The Truth About Marijuana 08/20/2018 |
pathway, heroin, opioid, video |
|
Opioid Use During Pregnancy 07/16/2018 |
opioid, Pregnancy, DFAF |
|
More Coloradans died last year from drug overdoses than any year in the state’s history. That shows how the opioid epidemic is changing. 07/03/2018 |
opioid |
|
Recreational Cannabis Legalization and Opioid-Related Deaths in Colorado, 2000-2015 05/13/2018 |
Note: If you look at the blue bar you will see that opioid deaths have more than quadrupled since medical marijuana was legalized in Colorado (in 2000). And deaths rose from 377 in 2012 (year mj legalized) to 504 in 2016. No evidence that legal marijuana is helping in Colorado- if anything it could be contributing to making the opioid epidemic worse! But the conclusion is not supported by data. This study and others that conclude marijuana helps fight the opioid crisis do not consider the many other strategies that have been implemented to fight opioid abuse, including the PDMP, treatment and Narcan. Nor is there any proof people are substituting marijuana for opioids. And this particular CO research (below) flies in the face of the actual data/ facts! Opioid deaths in Colorado have increased based on the data from Colorado Public Health and Environment Dept. Study's conclusion does not seem to match data.
opioid, Colorado |
|
SAMHSA Head Stands Firm on Marijuana's Dangers Also says younger generation of providers is key to opioid fight 04/26/2018 |
I'm here to tell you this is not a safe drug," McCance-Katz said during a town hall event at "NatCon18," the National Council for Behavioral Health's annual conference. McCance-Katz, SAMSHA, opioid |
|
Medical Marijuana Users are More Likely to Use Prescription Drugs Medically and Nonmedically 04/17/2018 |
Conclusions: Our findings disconfirm the hypothesis that a population-level negative correlation between medical marijuana use and prescription drug harms occurs because medical marijuana users are less likely to use prescription drugs, either medically or nonmedically. Medical marijuana users should be a target population in efforts to combat nonmedical prescription drug use. opioid, study, Research |
|
Big Marijuana moves to exploit the Opioid Epidemic 03/02/2018 |
Marijuana use is associated with an increased risk of prescription opioid use.
Drug Free America, opioid |
|
MARIJUANA, OPIOIDS, AND PAIN MANAGEMENT 02/01/2018 |
 “The opioid crisis appears to be worsening where marijuana has been legalized.” - JAMA INTERNATIONAL MEDICINE JOURNAL, 2018 opioids, opioid |
|
Cannabis Use and Risk of Prescription Opioid Use Disorder in the United States 01/01/2018 |
Conclusions:
Cannabis use appears to increase rather than decrease the risk of developing nonmedical prescription opioid use and opioid use disorder. opioid, psychiatryonline |
|
Treatment of acute cannabinoid overdose with naloxone infusion 11/01/2017 |
The overlapping endocannabinoid and endogenous opioid systems may explain this patient's response to therapy, and this synergistic relationship is discussed. opioid, synergistic |
|
Substance abuse rarely starts with opiate use on its own 09/02/2017 |
We therefore must educate our youngsters, parents and educators before any use of marijuana or alcohol begins. We then must identify those individuals for whom marijuana or alcohol use has become problematic, getting them into an effective program of treatment before they progress to more dangerous alternatives. School, opioid, opinion |
|
Opioid crisis declaration by President Trump welcomed in Florida 08/13/2017 |
The largest increases in opioid-related deaths in Florida from 2014 to 2015 were from the following drugs: Buprenorphine (up 102 percent), heroin (up 74 percent), fentanyl (up 69 percent), codeine (up 57 percent), and Oxymorphone (up 42 percent). opioid |
|
Benefits and Harms of Cannabis in Chronic Pain or Post-traumatic Stress Disorder: A Systematic Review 08/01/2017 |
"We found no observational studies that met inclusion criteria, but a growing body of cross-sectional literature suggests negative opioid-related correlates among individuals who use cannabis and opioids concurrently. These include opioid misuse;9,10,99,133 a greater number of opioid refills;99 a longer duration of opioid use; a higher dose of opioid medication prescribed;9 and endorsement of using opioids and other pain medications without a prescription.134" Veterans, opioid, study |
|
Cannabis Use and Risk of Prescription Opioid Use Disorder in the United States 04/26/2017 |
Cannabis use appears to increase rather than decrease the risk of developing nonmedical prescription opioid use and opioid use disorder. psychiatryonline, opioid |
|
Washington Poison Center Toxic Trends Report* 2016 Annual Opioid Report 03/03/2017 |
The Washington Poison Center (WAPC) saw a slight increase in calls regarding opioid exposures in 2016 (n=1,696) compared to 2015 (n=1,672). Of the calls received, over 70% (n=1,199) of the exposures occurred in individuals 20 years of age or older. 2016, Washington, opioid |
|
Mexican army faces uphill battle against opium poppies 12/31/2016 |
"Every time we destroy a field ... the locals come back to plant after our personnel has left the area," said Colonel Cipriano Cruz Quiroz, chief of staff of a special narcotics eradication unit based in Badiraguato, Sinaloa state. opioid, Mexico |
|
Cost of heroin epidemic tops $1 billion a year in Florida 12/22/2016 |
heroin, Florida, opioid |
|
MARIJUANA & OTHER DRUGS: A LINK WE CAN'T IGNORE 12/20/2016 |
SAM, opioid |
|
Marijuana and Opioid Conncection 10/16/2016 |
 Connection between legalization of marijuana and increase opioid addiction. Colorado, Pregnancy, opioid, video |
|
Relationship between Nonmedical Prescription-Opioid Use and Heroin Use 03/24/2016 |
Furthermore, the study shows that people engaged in the non-medical use of prescription opioids rarely use heroin. Also, the transition to heroin for people abusing prescription opioids occurs at a lower rate than for others. The research indicates that the primary causes in the increase in heroin use and associated overdoses are lower market prices and higher purity for heroin. opioid, heroin |
|
Number Using Opioids and Marijuana on the Rise 09/15/2015 |
"We found support for the synergistic effect on an individual level; people who tend to use more marijuana also tend to use more opioids," said Scott Novak, PhD, senior research scientist at RTI International, a leading research institute in Research Triangle Park, North Carolina. medscape, opioid, Studies, NSDUH |
|
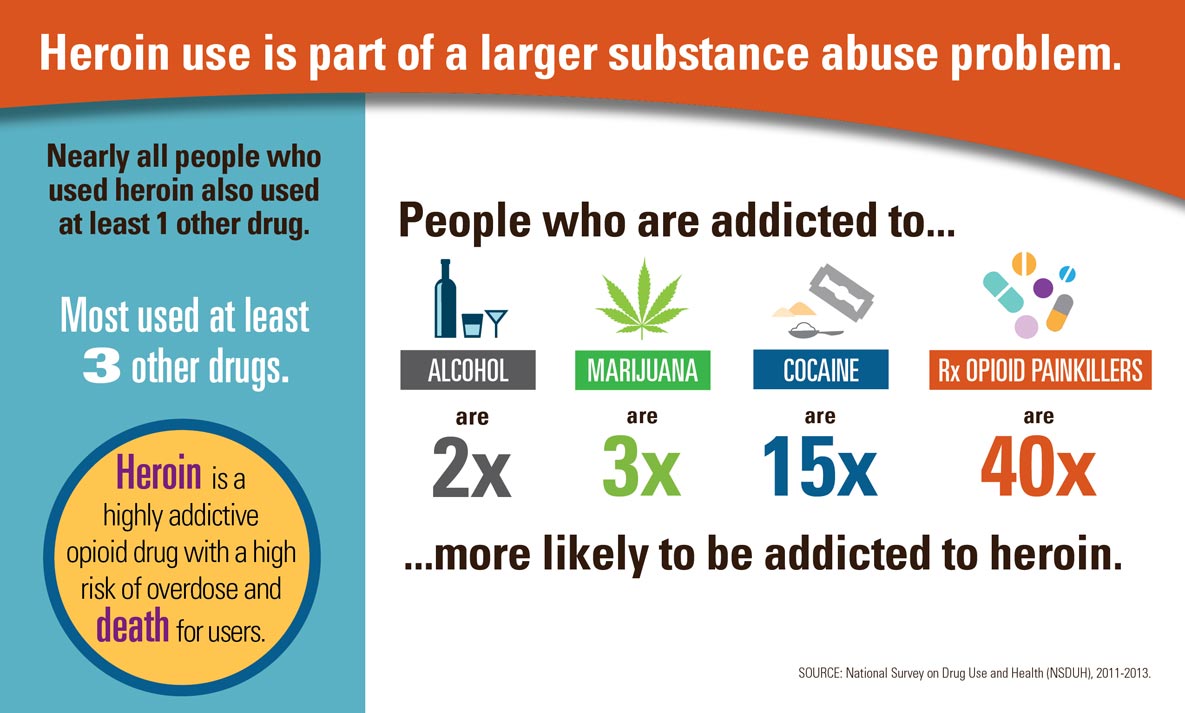
Today’s Heroin Epidemic Infographics 07/11/2015 |
|
|
Chart: Colorado among states with growing heroin, prescription drug abuse problem 01/28/2015 |
"Marijuana is the 800-pound gorilla in the room, when in fact, 295 Coloradans died two years ago of prescription drug overdoses," he notes. opioid, Colorado, legalization |
|
Drug czar: Teen pot use could fuel opioid abuse 10/11/2014 |
Teen, youth, opioid, abuse |
|
Marijuana- 2014 Dr. Madras Presentation 07/01/2014 |
madras, opioid, Pregnancy, youth, powerpoint, Brain |
|
Cannabis Use during Adolescent Development: Susceptibility to Psychiatric Illness 10/13/2013 |
adolescent, Psychiatric, addiction, Schizophrenia, opioid, Studies |